OkRx creates technology to connect specialty medication stakeholders from end-to-end.
We make it easier for Patients and their healthcare teams to navigate specialty medication coverage through centralized digital solutions.
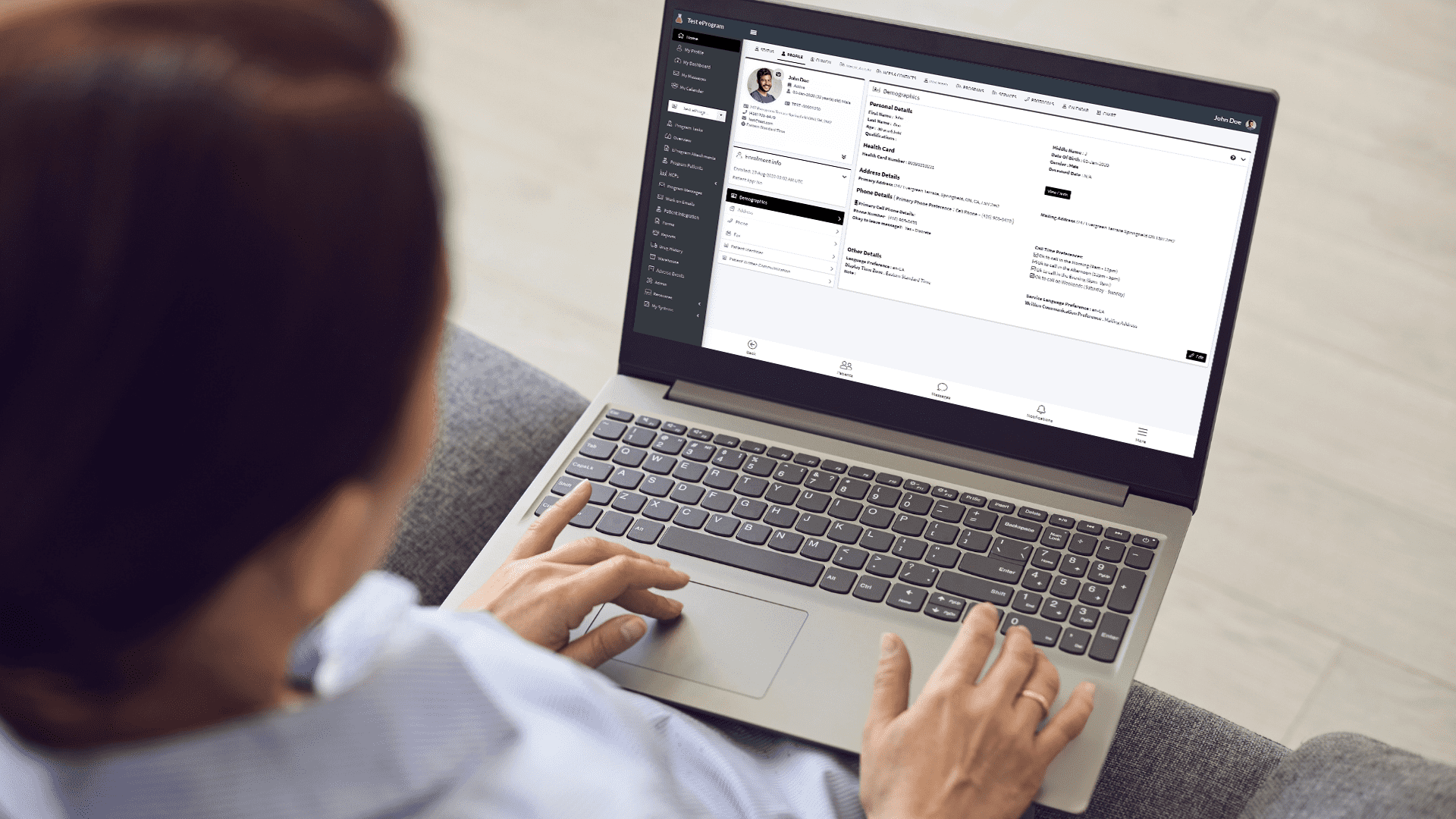
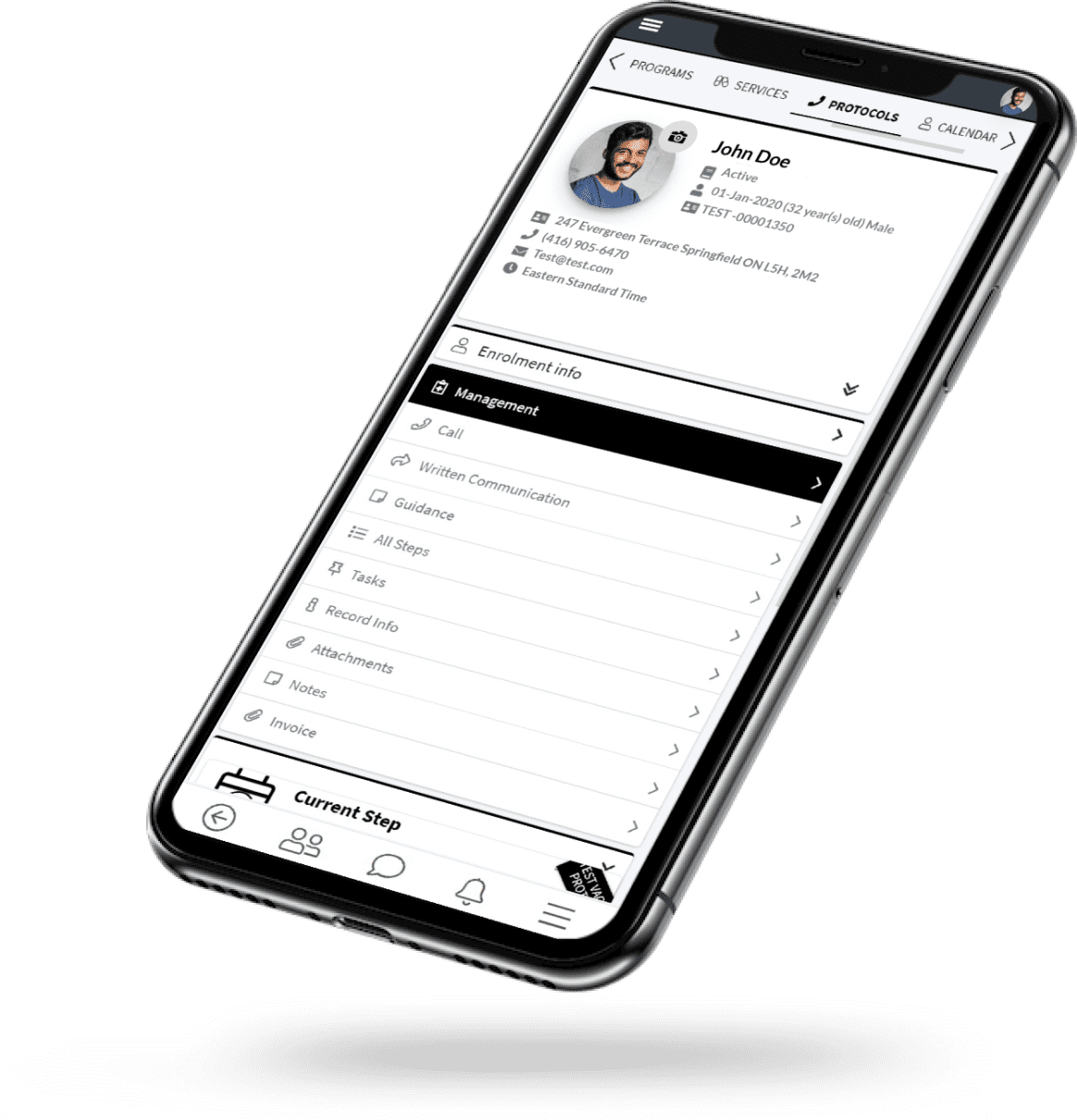
Patient Support Workflow
Built with the complexity of patient support in mind, OkRx ManageMedTM CRM allows you to meet the workflow demands of any regional or national specialty medication care offering or Patient Support Program (PSP).
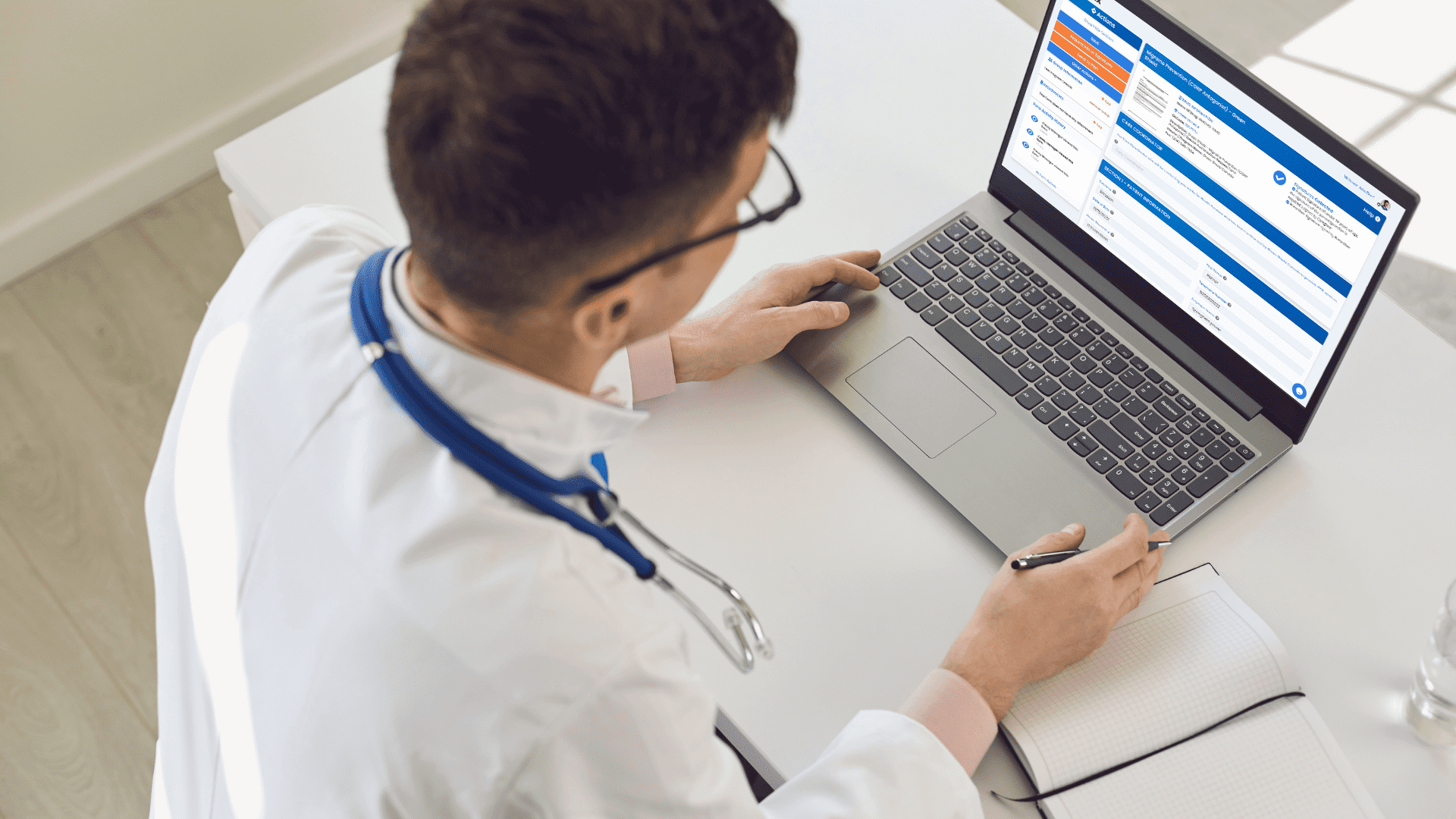
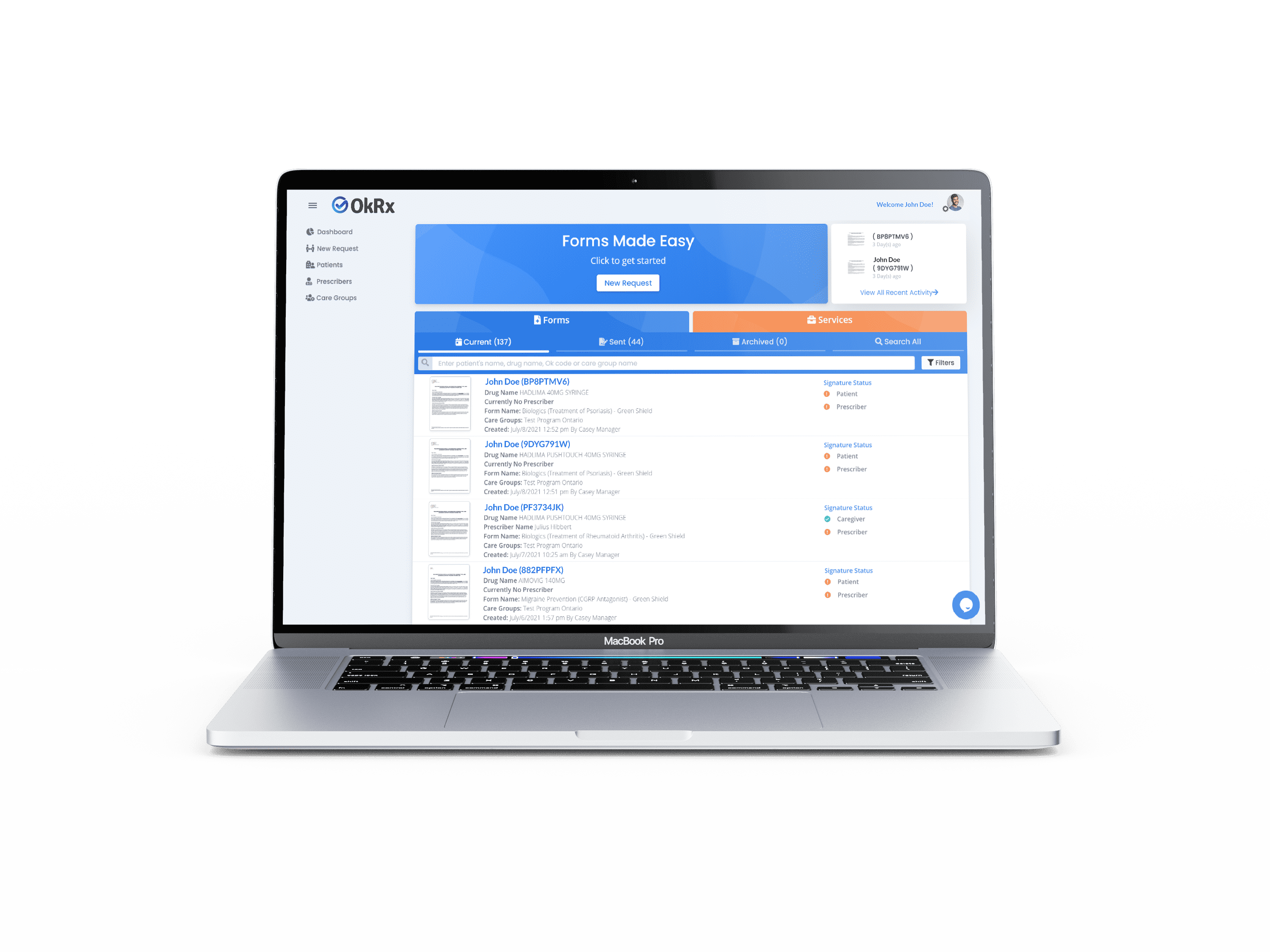
Learn More >Digital Forms
Providers can spend more time with patients and less on paperwork when they collaborate on drug Prior Authorization (PA) and Patient Support Program (PSP) enrolments forms digitally through a single online platform.
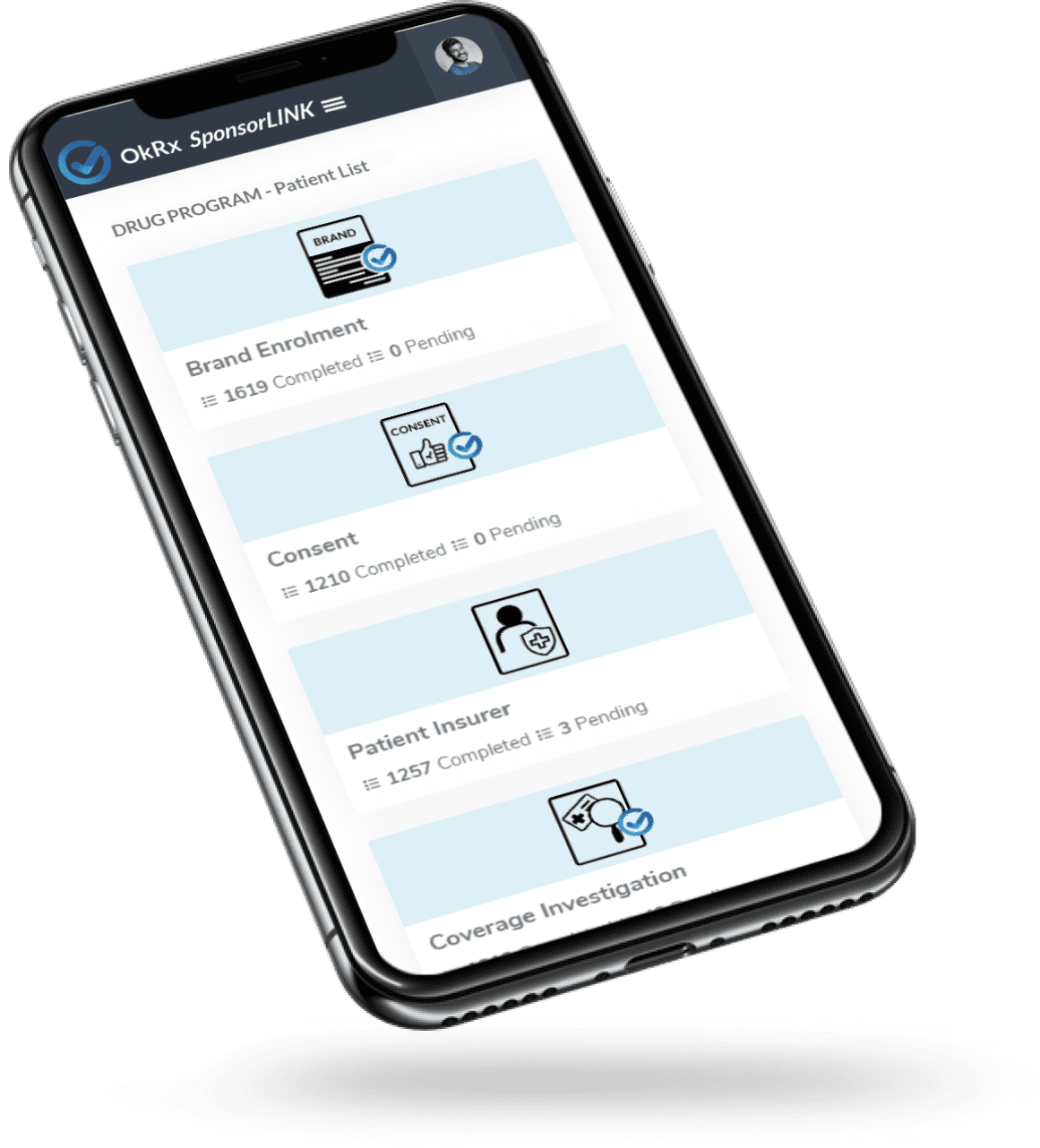
Learn More >Patient Engagement
Available on both iOS & Android devices, patients and their caregivers can enroll into services and communicate with their Patient Support Programs throughout the treatment journey.
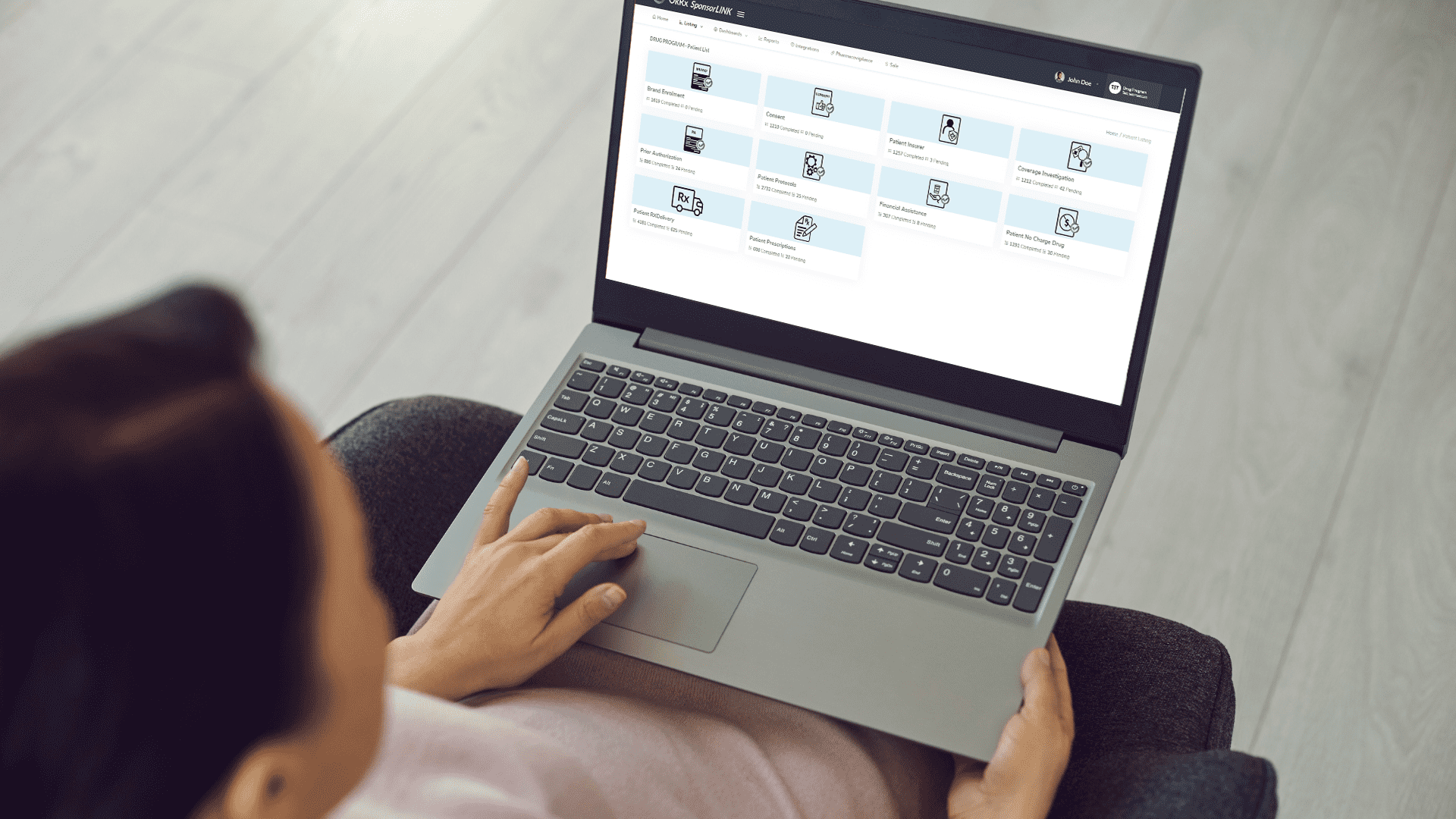
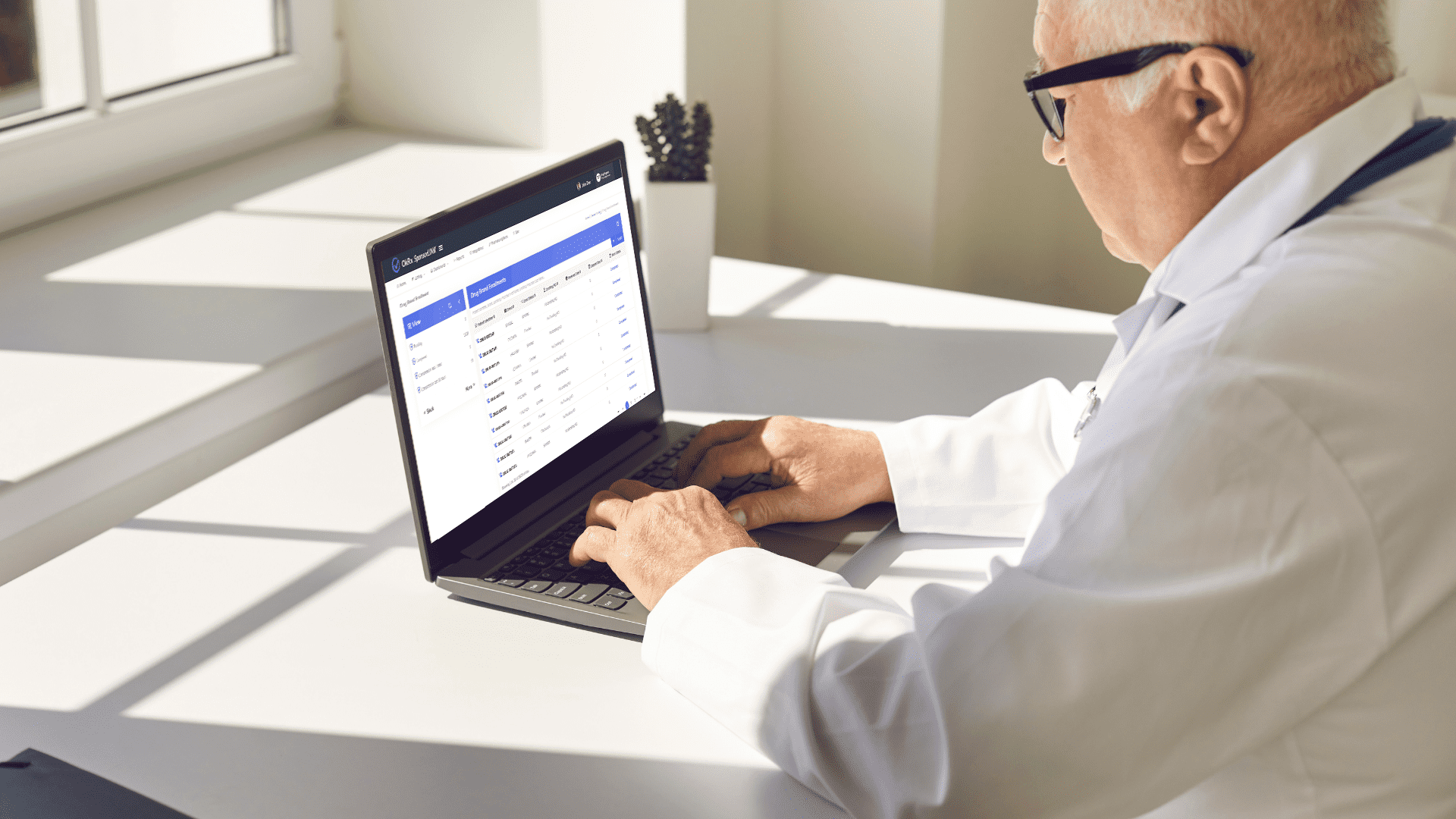
Learn More >Actionable Data Insights
Make the most informed decisions about your drug brands and their Patient Support Programs (PSPs) with real-time de-identified, patient-level data and business intelligence reporting.
Learn More >